
Images Ava Ghalini text Genevieve Carbonatto
A patient is referred by his GP to the Emergency Department for episodes of exertional upper chest pain over a period of 2 weeks. A troponin organised by his GP was 28. On arrival he is asymptomatic. BP 180/80, HR 100/min. A systolic and loud diastolic murmur is audible in the 2nd intercostal space.
A point of care ultrasound is performed
PLAX shows a dilated left ventricle with restricted MV opening. There is bouncing of the IVS

The LV measures 6.8 cm at end diastole (Normal 4.2 cm – 5.8 cm)
The aortic root and the sinus of Valsalva are dilated.
Colour Doppler shows moderate AR
The vena contracta is just over 65% of the LVOT indicating moderate to severe AR


The aortic annulus measures 2.2 cm (normal 2.6 +/- 0.3cm), the aortic root, 5.88 cm (normal 3.4 cm +/- 0.3 ) the proximal ascending aorta 5.81 cm (normal 3.0 +/- 0.4 cm)

The short axis view (SAX) shows a dilated LV, with mildly reduced LV contraction and bouncing of the IVS

The aortic valve leaflets are difficult to see clearly in the SAX view but the aortic valve appears trileaflet.
The 4 chamber view confirms the dilated LV and poor longitudinal contraction of the LV.
There is moderate to severe AR with colour Doppler
CW Doppler through the AV shows a dense AR signal. Compare this with the forward blood flow below the baseline. It is almost as dense as the AR signal.

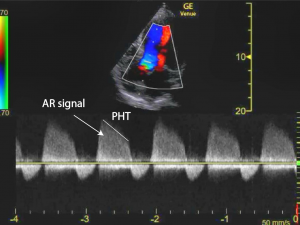
The pressure 1/2 time (PHT) is 240 ms ( PHT < 200 suggests severe AR)
In summary, he is found to have a moderate to severely dilated LV with mildly reduced overall systolic function. There is moderate to severe aortic regurgitation and severe dilatation of his aortic root.
A CT scan confirms an ascending aortic aneurysm with a normal aortic arch and descending aorta.
A formal ECHO confirms the aortic valve is trileaflet. Syphilis serology is negative.
He is referred for a bioprosthetic valve replacement which is organised within the next 24 hours.
Discussion
The incidence of thoracic aortic aneurysms is estimated to be 4.5 cases per 100 000.
Ascending aortic aneurysms can be divided into 2 categories : aortic root aneurysms which include the sinuses of Valsalva , and supravalvular aneurysms which do not involve the valves located above the sinus of Valsalva up to the brachiocephalic trunk.

The main concern of aortic aneurysms is that they are indolent and asymptomatic but associated with a high risk of rupture and dissection with catastrophic consequences.
- aortic root aneurysms are more common than supravalvular aneurysms
- the male: female ratio is 1:1 for aortic root aneurysms and 3: 1 for supravalvular aneurysms
Causes
| Congenital | Hereditary | Acquired |
| Bicuspid valve | CT tissue disease
· Marfan’s syndrome (20% will need an operation for an aortic root aneurysm) · Ehlers – Danlos syndrome · Leoys- Dietz syndrome
Familial aortic syndromes |
Hypertension
Infectious · Syphilis (now rare) · Bacterial (Infectious endo) · Viral · Fungal Autoimmune · Takayasu · Idiopathic aortitis Post traumatic Post surgery (eg at aortic suture line or at the site of aortic cannulation |
Age of complications from aortic root dilation is dependent on aetiology (2)
| Mean age at presentation (years) |
Source | |
|---|---|---|
| Hypertensive | 64.2 | (Davies, Kaple et al., 2007) [16] |
| Marfan syndrome | 24.5 | (Jondeau, Detaint et al., 2012) [17] |
| 34.4 (age at prophylactic surgery) | ||
| 39.4 (age at aortic dissection) | ||
| Bicuspid aortic valve | 49 | (Davies, Kaple et al., 2007) [16] |
| Familial (non syndromic) | 56.8 | (Albornoz, Coady et al., 2006) [18] |
| Loeys–Dietz syndrome | 19.8 (age at complications) | (Loeys, Schwarze et al., 2006) [8] |
| Ehlers–Danlos syndrome | No data |
The size of the aorta also influences the risk of rupture but the size at which complications occur is not the same for all aetiologies.
Diameter of ascending aorta and risk of complications. (2)
| Mean size at complications (mm)a | Source | |
|---|---|---|
| Hypertensive | 60 | (Davies, Kaple et al., 2007) [16] |
| Marfan syndrome | 51 | (Roman, Rosen et al., 1993) [19] |
| 56 | (Kornbluth, Schnittger et al., 1999) [20] | |
| 50–59 | (Jondeau, Detaint et al., 2012) [17] | |
| Bicuspid aortic valve | 52 | (Davies, Kaple et al., 2007) [16] |
| Familial (non-syndromic) | No data | No data |
| Loeys–Dietz syndrome | 40–50 | (Loeys, Schwarze et al., 2006) [8] |
| Ehlers–Danlos syndrome | No data | No data |
- When the aortic root reaches 5.5 cm
- If the growth rate exceeds 0.5 cm/year
- If the aortic root is 4.5 cm and the patient is going for another major cardiac surgery
For patients with Marfan’s syndrome or a bicuspid aortic valve
- When the ascending aorta reaches 5.0 cm
- when the aorta reaches 4.5 cm with a family history of complications or if the patient is going for an aortic valve replacement
- If there is significant AR and the ascending aorta is > 4.5 cm
- If the annual growth > 0.5 cm/year
Medical management
According to the ACC guidelines the aim is to control BP to reduce the risk of stroke, myocardial infarction, heart failure and cardiovascular death
- < 140 /90 in patients without diabetes
- < 130/80 in patients with diabetes or chronic renal disease
- Propranolol has been shown to reduce the rate of dilatation of the ascending aorta
- ACE inhibitors have also been found to slow the rate or aortic growth.
References
- Heart. 2006 Sep; 92(9): 1345–1352.doi: 10.1136/hrt.2005.074781PMCID: PMC1861150PMID: 16908722Dilation of the thoracic aorta: medical and surgical management
Patrick Nataf and Emmanuel Lansac - Int J Cardiol Heart Vasc. 2015 Mar 1; 6: 91–100.Published online 2015 Jan 20. doi: 10.1016/j.ijcha.2015.01.009PMCID: PMC5497177The ascending aortic aneurysm: When to intervene?
Emile Saliba,⁎ Ying Sia





