
Images Evy Panos, Text Genevieve Carbonatto
A 32 year old lady presents by ambulance to the Emergency Department in shock. She describes having felt dizzy but not unwell and then suddenly collapsed. She remembers being escorted in a wheelchair into an ambulance. She is 19 weeks pregnant and has had a recent normal ultrasound scan. Her BP on arrival is 65 mmHg systolic with a HR of 50 bpm. Fetal HR 60 bpm. She is drowsy, cold and clammy.
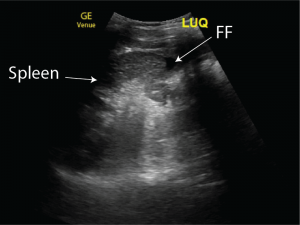
A point of care ultrasound is performed.
In the RUQ free fluid is present in Morison’s pouch. It is partially coagulated and therefore not all of it is anaechoic
A mixture of uncoagulated (white arrow) and coagulated blood (red arrow) is seen in the RUQ








There is a small amount of free fluid in the LUQ

Suprapubic transverse view
Laminated coagulated blood can be seen anterior to the bladder (red arrow – coagulated, white arrow uncoagulated)


Coagulated blood (red star) is seen in the POD. A sliver of uncoagulated free fluid is visible.


The patient is urgently transferred to theatre for a laparotomy with the surgeons and gynaecologist attending. She has 2.6l of blood in her peritoneum most likely originating from a right fallopian tubal mass. The mass is excised, the patient is resuscitated with 4 units of packed cells and recovers well. The intrauterine pregnancy is salvaged. Histopathology of the tubal mass confirms a right tubal ectopic pregnancy.
On further questioning, the patient reports miscarrying earlier in the year. An IUGS had been identified with a fetal pole but no heart beat at the time. This raised the possibility of this being either a heterotopic pregnancy or an old ectopic pregnancy.
Discussion
This case is unique as bleeding from the ectopic heterotopic pregnancy occurred at an intrauterine gestational age of 19 weeks. 70% of heterotopic pregnancies are diagnosed between 5 and 8 weeks of gestation, 20% between 9 and 10 weeks and only 10% after the 11th week.
- Heterotopic pregnancies are extremely rare – the incidence being around 1: 30,000 for naturally conceived pregnancies, 1-3:100 for pregnancies with assisted reproduction. The overall incidence being 1 in 4000 to 7000 pregnancies
- There has been an increase in incidence worldwide because of the increase in assisted reproduction, pelvic inflammatory diseases and improved ability to detect ectopic pregnancies. Other risk factors include previous pelvic surgery and previous ectopic pregnancies
- The ectopic gestational sac is most likely to be tubal, but cervical, ovarian and abdominal heterotopic pregnancies have been reported
- Most heterotopic pregnancies are from singleton intrauterine pregnancies but triplet and quadruplet heterotopic pregnancies have been reported
- Diagnosis is often missed because of the falsely reassuring intrauterine pregnancy
- Early diagnosis may be difficult without screening as the patient is asymptomatic.
- Heterotopic pregnancies present with four common presenting signs and symptoms, abdominal pain, adnexal mass, peritoneal irritation and an enlarged uterus. Abdominal pain has been reported in 83% and hypovolemic shock with abdominal tenderness reported in 13% of heterotopic pregnancies.
- When the patient does develop pain and an intrauterine pregnancy is visualised, patients may be misdiagnosed with adnexal torsion, hemorrhagic corpus luteum, ovarian cyst, tubo-ovarian abscess or appendicitis.
- A high index of suspicion is needed in patients presenting with a single intrauterine pregnancy and an abnormally high BHCG level even though the ultrasound may not show an adnexal mass.
- Heterotopic pregnancy should be considered in all patients with an intrauterine pregnancy presenting with acute lower abdominal pain, intra abdominal free fluid or shock
- The rate of death has decreased in developed countries due to increased ultrasound screening in early pregnancy but remains high in developing countries
- Management involves removal of the ectopic and conservation of the intrauterine pregnancy. The survival rate of the uterine foetus in heterotopic gestations is 70%
From the ultrasound point of view, the presence of coagulated blood misdiagnosed as bowel in the pelvis, or in this case liver tissue in the RUQ is always a diagnostic trap when scanning a patient with a ruptured ectopic pregnancy in the Emergency Department
References
- Annals of Clinical and Laboratory research : Management and Outcome of Heterotopic Pregnancy Han Li-Ping*, Zhang Hui-Min, Gao Jun-Bi, Tan Chao-Yue and Han Xiao-Xiao Department of Obstetrics and Gynecology, the First Affiliated Hospital of Zhengzhou University, Zhengzhou, P.R. China
- J Hum Reprod Sci. 2008 Jan-Jun; 1(1): 37–38.Heterotopic pregnancy in natural conception Govindarajan MJ and Rajan R
- J Emerg Trauma Shock. 2010 Jul-Sep; 3(3): 304.Heterotopic pregnancy: A diagnosis we should suspect more often Karim Ibn Majdoub Hassani, Abderrahim El Bouazzaoui,1 Mohammed Khatouf,1 and Khalid Mazaz





