Images and text Genevieve Carbonatto
An 88 year old woman presents to ED from a nursing home hypotensive. She has recently been admitted to hospital with pneumonia, CCF, AF and bilateral below knee DVT’s. She was discharged on warfarin. She is generally feeling tired, has abdominal pain and is vomiting coffee ground vomit.
On examination, her BP is 70/40, HR 80/min, saturations 90% on 6L of oxygen. There are bibasal crepitations on examination of her chest. She has a soft abdomen with a large, tender, firm mass in the RIF.
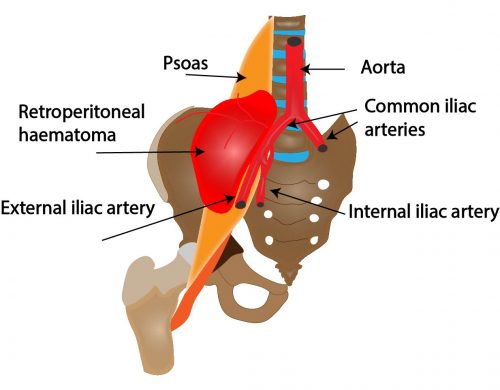
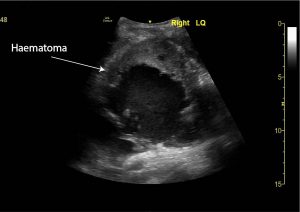
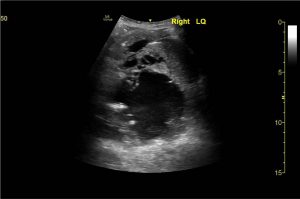
A point of care ultrasound is performed in on arrival. There is a large mass in the RIF which appears to have mixed echogenicity. Within the anechoic area, pulsatile blood can be seen entering the area.

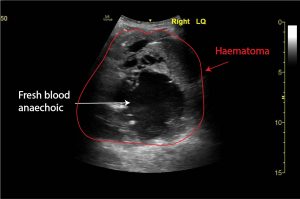
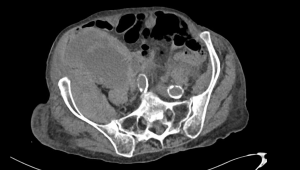
Her blood gas results return. Her haemoglobin is 66. Her lactate 6.1. A CT angiogram is immediately organised looking for a source of bleeding. In the meantime her INR returns at 3.3. Her CT scan shows a giant spontaneous right retroperitoneal haemorrhage with foci of active bleeding in the right iliacus muscle.

Her anticoagulation is reversed with vitamin K (10 mg) and prothrombinex. She is cross matched 6 units and she receives whole blood. She is transferred immediately to the angio suite where embolisation of multiple foci of haemorrhage in the right iliacus branches of the internal iliac artery is performed successfully.
She is transferred to ICU.
Unfortunately she rebleeds 6 days later and does not survive.
Discussion
This case illustrates the dangers of anticoagulation. Although rare, retroperitoneal bleeding is not uncommon and more frequently found in the context of anticoagulation. The elderly are more vulnerable. Bleeding can occur with therapeutic doses of anticoagulation therapy (3). If actively bleeding, management centers on cessation of anticoagulation, antocoagulation reversal, volume resuscitation with transfusion therapy and haemodynamic stabalisation.
Causes of retroperitoneal haematoma (spontaneous vs secondary)
1. Spontaneous haematomas.
Risk factors:
- Anticoagulation . The INR may still be in the therapeutic range for a retroperitoneal bleed to occur.
- Hypertension (33 -50%)
- Atherosclerosis (80 -87%)
- Age > 65
- Coagulopathies
- Haemodyalisis
- Diabetes mellitis
2. Iatrogenic/trauma/ underlying pathology
- Iatrogenic : Post femoral artery catheteriusation
- Pelvic lumbar trauma
- Ruptured AAA
- Bleeding from the kidneys (2 to a renal cell carcinoma, angiomyolipoma) or adrenal glands ( adrenal myelolipoma, phaemochromocytoma, adrenal hemangiomas )
- Vascular abnormalities of the kidneys or adrenal glands (e.g. necrotizing arteritis, connective tissue diseases,ruptured visceral artery anerysm)
Pathogenesis:
The true pathogenesis of spotaneous retroperitoneal bleeding is unknown. It is possibly due to retroperitoneal microvascular atheroslerosis causing the vessels to rupture with involvement of proximally large vessels if stretched by the enlarging haematoma.
Clinically presentation:
- Acute abdominal/flank pain 67%
- Haematuria 40%
- Shock 26.5%
- Upper and lower quadrant tenderness to palpation
- Palpable mass
- Abdominal compartment syndrome (intraabdominal hypertension, renal failure)
- Anaemia
- Cutaneous signs rarely – Cullen’s sign (umbilical eccymosis) and Grey – Turner’s sign (flank eccymosis)
- Psoas haematomas can present with constipation, urinary frequency, compressive femoral neuropathy or fever if large
Diagnosis :
- CT scan – to confirm size, compressive complications and active bleeding (blush on CT)
- US may be useful in ED
Treatment :
- Resuscitate
- Reverse anticoagulation
- If on warfarin , Vitamin K 5 -10mg, Prothrombic X 20mg/kg, FFP ,platelets
- Replace blood loss – Blood transfusion,
- Intra-arterial embolisation of points of active bleeding
- Transfer to ICU
References
- Life in the fast lane Retroperitoneal haemorrhage by Chris Nickson
- Radiopaedia : Spontaneous retroperitoneal haemorrhage Dr Tim Luijkx and Dr Avni K P Skandhan et al.
- J Med Case Reports. 2008; 2: 162. Gigantic retroperitoneal hematoma as a complication of anticoagulation therapy with heparin in therapeutic doses: a case report
Stavros I Daliakopoulos,corresponding author1 Andreas Bairaktaris,1 Dimitrios Papadimitriou,2 and Perikles Pappas2 - J Surg Tech Case Rep. 2011 Jan-Jun; 3(1): 8–9. Spontaneous Retroperitoneal Hematoma: A Rare Devastating Clinical Entity of a Pleiada of Less Common Origins
Stavros I. Daliakopoulos - Ilio-psoas hematoma in the intensive care unit: a multicentric study J. F. LlitjosEmail author, F. Daviaud, D. Grimaldi, S. Legriel, J. L. Georges, E. Guerot, J. P. Bedos, J. Y. Fagon, J. Charpentier and J. P. Mira Annals of Intensive Care20166:8
- BMJ Case Rep. 2013; 2013: bcr2013201291. Case Report Emergency department ultrasound diagnosis of spontaneous iliopsoas haemorrhage in a patient on warfarin
Devesh Sharma,1 Ramy Saker,2 and Abha Govind - Intra-abdominal hypertension due to heparin – induced retroperitoneal hematoma in patients with ventricle assist devices: report of four cases and review of the literature
Stavros I Daliakopoulos,corresponding author1 Manja Schaedel,1 Michael N Klimatsidas,2 Sotirios Spiliopoulos,1 Reiner Koerfer,1 and Gero Tenderich





