The answers to this quiz can be found in the ASE quantification chamber guidelines 2018
1.What windows do you use to assess RV size ?
Use multiple windows including:
- Parasternal long-axis view (PLAX)
- Parasternal short-axis view (PSAX)
- Parasternal RV inflow view
- Apical 4-chamber view
- Focused apical 4-chamber RV view
- Subcostal view
Measurements are made inner edge to inner edge
The values are not indexed to gender, BSA or height.



RV linear dimensions are dependent on probe rotation and different RV views, so the report should state the window from which the measurement was obtained. A single measurement may not reflect global RV size.
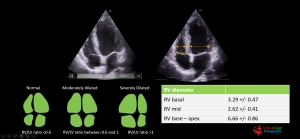
2. What RV diameter is considered normal at the base and at the mid level of the RV in the 4cV?
- Base : 41 mm
- Mid level : 35 mm
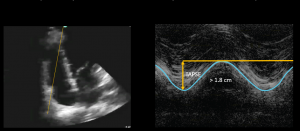
3. What is an abnormal RV wall thickness ?
- > 5mm is abnormal
- Measure using subcostal view zooming onto wall

4. How can you assess global RV function?
- TAPSE (tricuspid annular systolic excusion) is used to assess RV longitudinal contraction but has good correlation with parameters estimating RV global systolic function
- TAPSE measures the peak distance travelled by this reference point during systole by placing an M mode through the lateral annulus of the TV
- A greater distance travelled during systole implies greater RV systolic function
- Normal TAPSE > 17mm. If the TAPSE is less than 17mm then the longitudinal contraction of the RV is reduced
- TAPSE may over- or underestimate RV function because of cardiac translation. Translation motion occurs when the heart moves in a single direction that is not in the imaging plane.
- The primary limitation of TAPSE is that it only represents one component of RV motion within one single segment of RV myocardium. The RV may be frankly dysfunctional despite relatively preserved TAPSE, as in some cases of severe pulmonary arterial hypertension
5. What is defined as pulmonary hypertension?
Pulmonary hypertension is defined as an increase in mean pulmonary arterial pressure of > 25mmHg
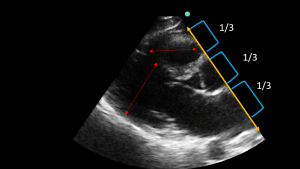
6. How would you assess the RV in the PLAX view?
The rule of thirds states that the size of the RV , the aorta and the LA should be approximately the same in the PLAX. If the RV is larger than the aorta and LA o larger than the LV then there is likely an increase in size of the RV
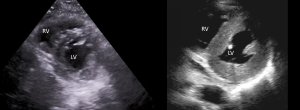
7. How would you assess the RV in the PSAX view?
In the PSAX view, if the LV appears D shaped (flattening of the interventricular septum) then this signifies RV strain or increased pressure in the RV
The first picture shows a normal round LV, the second a D shaped LV due to pulmonary hypertension
8. How would you assess the RV in the 4 chamber view ?
The RV size can be assessed by comparing it to the LV size.
If the RV is the same size as the LV then it is moderately dilated . If it is bigger than the LV it is severely dilated
9. In which views is it possible to obtain a tricuspid regurgitant signal using colour Doppler?
- Parasternal long axis (right ventricular inflow – pan down from PLAX)
- PSAX
- Apical 4cV
10. How do you measure right ventricular pressure from the tricuspid regurgitation velocity?
- Identify the TR jet with colour Doppler
- Place a CW Doppler through the jet to obtain a signal which has a satisfactory envelope.

- The maximum velocity of the TR jet is obtained ( above TR Vmax 2.64m/s)
- The machine will convert this into a maximum pressure gradient using the Bernouilli equation which is the relationship between velocity and pressure such that Δ P = 4 V² in the case above 27.93 mm Hg
To get a correct reading
- The CW Doppler line should be placed through the origin of the jet as in line as possible to the flow of blood
- If a jet is not clearly visible, get the patient to stop breathing and try to measure in inspiration ( TR is greatest during inspiration). Often cardiac views are best in held expiration so this may be a challenge
- If there is marked sinus arrythmia then measure in apneic expiration
- If the patient is in atrial fibrillation take an average of at least 3 readings
Pitfalls
- When there is severe TR, there may be rapid equalisation of pressures between the RV and the RA so the TR signal may be cut short leading to an underestimation of the PASP
- Calculations using the TR trace assumes there is no pulmonary artery valve stenosis
- This calculation is only possible if there is a good TR trace envelope.
11. How do you obtain the pulmonary artery systolic pressure ?
- Estimation pulmonary artery systolic pressure (PASP) uses a derivation of right ventricular pressure from the tricuspid regurgitation (TR) velocity (see above question) added to a qualitative assessment of right atrial pressure (RAP)
- The RAP is estimated by looking at the size and collapsibility of the IVC
| Variables | Normal (0 -5 (3) mm Hg | Intermediate (5-10(8) mm Hg) | High (15mm Hg) |
| IVC diameter | ≤ 21 mm | ≤ 21 mm; > 21 mm | > 21 mm |
| Collapses with sniff | > 50% | < 50%; > 50% | < 50% |
Ranges are provided for low and intermediate categories, but for simplicity, midrange values of 3 mm Hg for normal and 8 mm Hg for intermediate are suggested. Intermediate (8 mm Hg) RAPs may be downgraded to normal (3 mm Hg) if no secondary indices of elevated RAP are present, upgraded to high if minimal collapse with sniff (< 35%) and secondary indices of elevated RAP are present, or left at 8 mm Hg if uncertain. IVC: inferior vena cava; RAP: right atrial pressure. The table synthetically displays the concepts expressed by Rudski et al [19] in the official recommendations of the American Society of Echocardiography (2010). These criteria have been left unchanged in the recent update [20] (January 2015)
12. How do you measure the pulmonary acceleration time?
- Using colour Doppler obtain a regurgitant PR signal from the PSAX view
- Place a PW Doppler beam through the PV with the sample volume just proximal to the pulmonary valve in the RVOT
- The measurement is taken from the baseline to the peak velocity
- A value of > 130 ms is normal
- A value of < 100ms is suggestive of pulmonary hypertension

Pitfalls
- To get a correct result the Doppler beam has to be correctly aligned
- Heart rates outside the normal range (<60 or >100/min) may reduce the accuracy of the technique
- When the PAP exceeds 25 mmHg, the acceleration time is accurate even in tachycardia
10. What is the 60/60 sign?
This refers to a RV systolic pressure (RVSP) of less than 60 mmHg and a pulmonary acceleration time (PAT) of less than 60 msec. This has been found to be 94% specific and 36% sensitive in diagnosing PE. High RV pressures (>60mmHg) can only be generated in the context of chronic pulmonary hypertension. In the context of acute pulmonary hypertension pressures, because the RV wall has not had time to hypertrophy, high RV pressures cannot be generated.

Pitfalls
- The 60/60 sign is useful when it is either acute or chronic pulmonary hypertension. In the case of mixed cause of pulmonary hypertension (patient with underlying pulmonary hypertension and an acute PE) it is impossible to exclude a PE using the 60/60 sign.
13. What are the ECHO signs of an acute submassive PE?
- RV dilatation ( > 1/3 of LV in 4cV)
- IVS flattening causing a D shaped ventricle in the PSAX view
- TAPSE < 17 mm
- Pulmonary artery systolic pressure < 60 mmHg, pulmonary acceleration time (PAT) < 60 ms
- RV wall thickness < 5 mm
- McConnell’s sign
- proximal pulmonary artery dilation > 2.5 cm
- thrombus in IVC, RV, RA or Pulmonary arteries
- fixed and dilated IVC
Estimation of Pulmonary artery systolic pressure (PASP) uses a derivation of right ventricular pressure from the tricuspid regurgitation (TR) velocity added to a qualitative assessment of right atrial pressure (RAP)
14. What are the ECHO signs of chronic severe pulmonary hypertension?
- RV dilatation >1/3 of LV in 4cV
- IVS flattening in systole/diastole or both causing a D shaped ventricle in the PSAX
- TAPSE < 17mm
- Pulmonary artery systolic pressures > 60mmHg, Pulmonary acceleration time (PAT) > 60 ms but may be < than 60ms if severe
- RV wall thickness > 5 mm
- Mcconnell’s sign may be present
- Fixed and dilated IVC
Estimation Pulmonary artery systolic pressure (PASP) uses a derivation of right ventricular pressure from the tricuspid regurgitation (TR) velocity added to a qualitative assessment of right atrial pressure (RAP)
References
- J Clin Med Res. 2016 Aug; 8(8): 569–574.Published online 2016 Jul 1. doi: 10.14740/jocmr2617wPMCID: PMC4931801PMID: 27429676
Estimating Right Atrial Pressure Using Ultrasounds: An Old Issue Revisited With New Methods Renato De Vecchis,a,e Cesare Baldi,b Giuseppe Giandomenico,c Marco Di Maio,d Anna Giasi,a and Carmela Cioppaa - Int J Cardiol Heart Vasc. 2016 Sep; 12: 45–51.Published online 2016 Jul 4. doi: 10.1016/j.ijcha.2016.05.011PMCID: PMC5454185PMID: 28616542
Assessment of pulmonary artery pressure by echocardiography—A comprehensive review
Sathish Parasuraman,a,⁎ Seamus Walker,b Brodie L. Loudon,a Nicholas D. Gollop,a Andrew M. Wilson,a Crystal Lowery,a and Michael P. Frenneaux - A sonographer’s guide to the Assessment of Heart disease:Bonita Anderson
- GUIDELINES AND STANDARDS Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults:An Update from the American Societyof Echocardiography and the European Association of Cardiovascular Imaging




