Questions Robyn Boman/Genevieve Carbonatto
- What is the normal heart rate range for 1st trimester pregnancy at 6 weeks, 9 weeks and after 9 weeks and how would you measure it?
- At 6 weeks : 100-120 bpm
- At 9 weeks :140 -160 bpm
- ongoing average 140 bpm
- Measurement is made using M mode (motion mode) which displays time along the horizontal axis and depth long the vertical axis to depict movement to graphically represent movement


2. Discuss the reasons for not using colour Doppler or power Doppler in the 1st trimester.
Red cells scatter ultrasound poorly compared to tissues. To get an adequate Doppler signal, the machine increases it’s transmission power of the ultrasound beam. Pulse wave (PW) Doppler also relies on a single line of sight of the ultrasound beam which is stationary. This means that all the transmitted ultrasound energy travels along a single beam, exposing a small volume of tissue to a concentrated higher energy ultrasound beam. This energy is transformed into heat.
It is unclear whether there are any bioeffects of ultrasound , but in the developing fetus, in the first trimester it is best to use as little energy as possible when scanning. This principle is referred to as ALARA (As Low As Reasonably Achievable).
Reference: The Physics and Technology of Diagnostic ultrasound Dr Robert Gill
3. Describe the sonographic appearance of a subchorionic haemorrhage in a first trimester pregnancy.
- A subchorionic haemorrhage is the commonest site of bleeding within the early gestational sac and is a crescent shaped echo free area between the chorionic membrane and the myometrium.


The appearance of the blood depends on the age of the haematoma.
- Acute haemorrhage will be echogenic and particulate
- Older haemorrhages will become more anechoic
The size of the subchorionic haematoma is graded according to the percentage of the chorionic cavity elevated by the haematoma
- small <1/3
- moderate 1/3 – 2/3
- large > 2/3
Reference :Clinical ultrasound Paul Allen 3rd edition Elsevier
4.What is the name of a sac like structure which mimics a gestational sac when an ectopic pregnancy is present? How can it be distinguished from a true gestational sac?
- The name of the sac like structure found within the uterine cavity is called a pseudosac or pseudogestational sac.
- The term ” pseudogestational sac” or pseudo sac” is not a sac at all but simply intrauterine cavity fluid which may confuse the scanner into thinking it is a true gestational sac in the presence of an ectopic pregnancy. It occurs in approximately 10% of ectopic pregnancies.
- It can be distinguished from a true gestational sac by
| Pseudogestational sac | True gestation sac |
| There is a single echogenic rim surrounding the intrauterine fluid. This can be a thick decidual reaction | A gestation sac has 2 hyperechoic rings consisting of an outer and inner ring, the decidua vera and the decidua capsularis |
| Located centrally inside the uterine cavity | Eccentrically located |
| Shape may be irregular and changes during the scan. Usually ovoid | Steady, round shape |
| Avascular | High peripheral vascular flow |
| Absence of fetal pole or yolk sac | Presence of fetal pole and fetal yolk sac |
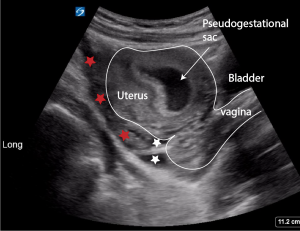
Below images show a pseudogestational sac, coagulated blood (red stars) and non coagulated blood (white stars) surrounding the uterus in a patient with a rutured ectopic pregnancy.



5. What factors may increase the likelihood of developing a heterotopic pregnancy?
There has been an increase in incidence worldwide of heterotopic pregnancies because of
- an increase in assisted reproduction
- an increase in pelvic inflammatory diseases
- improved ability to detect ectopic pregnancies
Patients are also at risk if they have had
- previous pelvic surgery
- previous ectopic pregnancies
6. What are potential locations for ectopic pregnancies.
- Tubal (interstitial and cornual, isthmic, ampullary, fimbrial
- Ovarian
- Cervical
- Peritoneal/abdominal
- Caesarian scar

7. What is the earliest parameter that can be used to establish gestational age and how is it measured?
- Measurement of the MGSD (mean gestational sac diameter) is the first parameter that can be used to establish gestational age.
- It is measured by using split screen, identifying the gestational sac in both the transverse and longitudinal view and measuring the diameter in height, width and length


- The rate of growth of the gestational sac is 1.1 mm/day
Reference :Clinical ultrasound Paul Allen 3rd edition Elsevier
8. At what MGSD should an embryo be visible using transabdominal US?
An embryo should be visible on TA ultrasound when the MGSD is 25mm. If the embryo is not visible it is highly suggestive of a failed pregnancy
Reference :Clinical ultrasound Paul Allen 3rd edition Elsevier
9. At what gestational age should an intrauterine gestational sac be visible on a transabdominal scan? At what gestational age should the fetal pole be visible on a transabdominal scan?
A gestational sac should be visible using transabdominal ultrasound at a gestational age of 6 weeks and the fetal pole and cardiac activity by 7 weeks.
This compares with the gestational sac being visible using transvaginal ultrasound by 4 weeks and the fetal pole and heart beat between 5 and 6 weeks

10. At what level of BHCG should a gestational sac be visible on transabdominal ultrasound?
The discriminatory zone is defined as the BHCG level above which an imaging scan should reliably visualize a viable intrauterine pregnancy. It is 6000 IU/ml for TAS. However, visualisation of the gestational sac depends on factors such as the scan resolution (type of machine used), the body habitus of the patient (obesity makes visualisation difficult), the position of the uterus ( much harder to see the fundus in a retroverted uterus if the bladder is not full), and the skill of the operator.
If the an IUGS is not visible then a transvaginal scan should be performed.





Very informative
Thankyou Donna Marie!