
Images : Sarah Vaughan, text Genevieve Carbonatto
A 56 year old man presents to the Emergency department short of breath and unwell. He gives a history of 2 hours of shortness of breath and chest pain. He has been recently diagnosed with metastatic adenocarcinoma.
These are his vital signs

He is hypotensive, his BP arterial trace showing electrical alterans, and his ECG complexes on the screen are small. He is also hypoxic at room air. On examination his chest is clear, his HS are dual but muffled, his RR is 30/min.
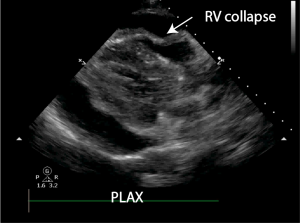
A point of care ECHO is performed. A large pericardial effusion is present, there is swinging of the heart. RV collapse is best seen in the PLAX view, RA collapse is best viewed in the 4CV. The IVC is fixed and dilated. A pericardiocentesis kit is opened at the bedside. He is given 1l of normal saline iv. This improves his BP and he manages to go straight to the catheter lab for a pericardiocentesis.



Discussion:
We have, in a previous post, discussed the ECHO features suggestive of tamponade. These include
- RA wall collapse – in early systole or late diastole. If more than 1/3 of the cardiac cycle then this is almost 100% specific and sensitive for clinical cardiac tamponade
- RV wall collapse – in diastole. First only in expiration then throughout the cardiac cycle. The longer the indentation of the free wall, the more significant the severity of the haemodynamic compromise
- LA collapse – usually seen with RA collapse. Not common
- LV wall collapse – unusual – seen in patients with severe pulmonary hypertension
- Swinging heart
- IVC is fixed and dilated in cardiac tamponade, unless the patient is severely dehydrated. This has been termed “low pressure cardiac tamponade” and BP can be improved with iv fluids
In this patient RA and RV collapse are demonstrated. The heart is swinging. Irrespective of the cardiac ECHO findings, the presence of a pericardial effusion in a patient who is clinically haemodynamically compromised indicates pericardial tamponade. This is a life threatening condition, for which urgent pericardiocentesis is indicated. Giving a bolus of fluid may improve RV filling. This man did receive 1l of normal saline which improved his BP to 110 systolic and gave him enough time for a drainage to be done in the cardiac catheter lab. 700 mls of serosanguinous fluid was drained. The size of the effusion does not determine whether pericardial tamponade is present. The pericardium will be able to accommodate more fluid in a chronically enlarging effusion and may cause tamponade when the effusion is very large, tamponade may occur with much less volume of fluid if the effusion accumulation is acute.

Teaching point: The diagnosis of pericardial tamponade is a clinical diagnosis where haemodynamic instability is due to the presence of pericardial fluid.





