A 45 year old patient presents in cardiac arrest . What is the ultrasound approach to this patient?
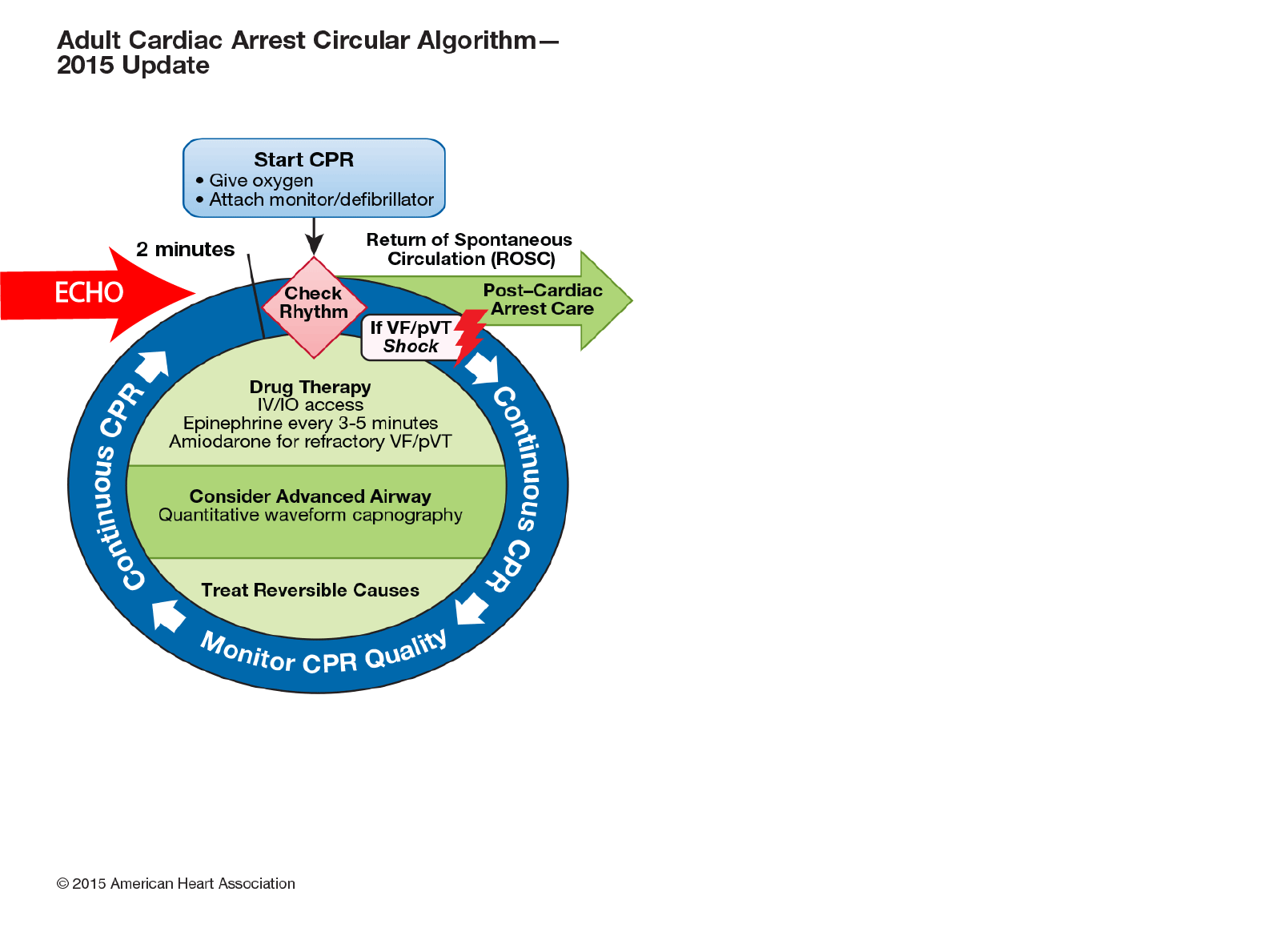
The approach to the patient in cardiac arrest is based on assessment of the 4 F’s (fluid, form, function and filling) of the heart to assess for potentially reversible causes of cardiac arrest, to assess prognosis and to guide treatment(1)
Approach:
Preparation
- Brief team
- Prepare ultrasound machine :
- Assign team member to machine
- Operator enters patient details (temporary ID or patient details if known, otherwise enter cardiac arrest ) into machine
- Operator enters his details into the machine
- Chose probe (sector), abdominal probe in adults or linear probe in children, adjust depth to 25 cm for initial subxiphoid view.
- Ensure that the scan operator knows whether the machine is saving prospective or retrospective loops.
Scanning
Stepwise clinical indication approach with core, supplementary and additional views
A. Core views : To be completed in all cardiac arrests
Basic cardiac windows
- Subxiphoid and/or
- PLAX windows
Search for
- Pericardial fluid : ? tamponade (RV collapse, swinging heart)
- Cardiac form : Is the heart small ( hypovolaemia ?), normal or large (cardiomyopathy ?) Is the RV larger than the LV (PE ?)
- Ventricular function : Is there vigorous contractility ( hypovolaemia ?) Is there no myocardial contraction (very poor outcome) ?Are the valves opening?
Basic cardiac windows are :
- Performed during rhythm check pause in chest compressions. Press record clip during this time.
- Reviewed whilst cardiac compressions are continuing
- Findings are related to the team leader during cardiac compressions.
B. Supplementary views : To be completed if time permits
1. Additional chest views :
- PSAX
- 4CV
2. Lung views
- Absent lung sliding (tension pneumothorax ?). Check by looking for lung pulse and make sure the patient is being ventilated before assuming pneumothorax present
- Pleural fluid
- B lines bilaterally (pulmonary oedema)
- B lines unilaterally suggesting consolidation due to inflammation
3. IVC
- Filling status : Is the IVC dilated and non-collapsing (usual in cardiac arrest) Is the IVC small and collapsing (hypovolaemia)?
C. Additional views as clinically indicated
- Confirmation of ET placement (double tract sign suggestive of oesophageal intubation, absent lung sliding in ventilated patient)
- Look for sources of blood loss ie peritoneal fluid (AAA, ruptured ectopic , peritoneal fluid). This should be performed in patients presenting with abdominal pain, +ve pregnancy test or patients on anticoagulation
- Aortic views for AAA or dissection if patient presents with abdominal or back pain or with history of vascular disease
- DVT In proximal deep veins of the legs and ilieofemoral veins
Operator during arrest saves cineloops, positions probe during CPR if possible to set view so that it is ready for scanning during the rhythm check
Reference
- International Federation for Emergency MedicineConsensus Statement: Sonography in hypotension and cardiac arrest (SHoC): An international consensus on the use of point of care ultrasound for undifferentiated hypotension and during cardiac arrest Paul Atkinson, MB, MA*†; Justin Bowra,MB‡§; James Milne, MD¶; David Lewis, MB*†; Mike Lambert,
MD**; Bob Jarman, MB, MSc†††‡‡; Vicki E. Noble, MD§§¶¶; Hein Lamprecht, MB***; Tim Harris,




